Journal of Case Reports and Reviews in Medicine (ISSN: 3069-0749)
Case Report Volume: 1 & Issue: 4
Case Report Volume: 1 & Issue: 4
Background: Extraskeletal Ewing sarcoma (EES) is a rare soft-tissue tumor with aggressive behavior and poor prognosis, especially when metastasized. Primary cutaneous manifestations are extremely uncommon.
Case Presentation: We report a case of a 22-year-old pregnant woman presenting with infraumbilical subcutaneous nodules that rapidly progressed postpartum. Histopathology confi rmed EES. Imaging revealed widespread metastasis to the breasts, lungs, liver, bones, and brain. Due to systemic involvement, palliative chemotherapy and radiotherapy were initiated but patient could not bear the disease and treatment burden and unfortunately died after 6 months.
Conclusion: This case highlights an aggressive presentation of EES with rare metastatic spread, underscoring the need for early suspicion and the role of imaging in guiding management.
Keywords: Extraskeletal Ewing Sarcoma, Breast Metastasis, Brain Metastasis, Cutaneous Manifestations, Chemotherapy
Ewing sarcoma is an aggressive malignant tumor arising from primitive neuroectodermal cells, predominantly aff ecting children and adolescents. Although primarily osseous, approximately 20– 30% of Ewing sarcoma cases present in soft tissues without bone involvement, known as Extraskeletal Ewing Sarcoma (EES).1
Cutaneous or subcutaneous manifestations of EES are exceptionally rare and can lead to diagnostic delays due to their benign appearance. EES exhibits rapid tumor growth and a high potential for systemic dissemination, which contributes to its poor prognosis.2
Only a limited number of EES cases with widespread metastasis have been reported in the literature. Imaging plays a pivotal role in diagnosis, staging, and treatment planning. Therapeutic strategies typically involve multimodal approaches, including chemotherapy, radiotherapy, and surgical excision.3
We report an unusual case of cutaneous EES in a young pregnant female with extensive metastases to uncommon sites including the breast and brain, emphasizing the importance of radiological evaluation in guiding clinical decision-making.
A 22-year-old female presented with multiple infraumbilical subcutaneous nodules that initially appeared during her fi rst pregnancy. These nodules progressively enlarged postpartum, accompanied by the development of bilateral breast masses, persistent bone pain, headaches, visual disturbances, and leftsided exophthalmos.
Initial dermatologic evaluation presumed benign skin lesions. However, due to progressive enlargement, a biopsy was performed. Histologically, the tumor displayed sheets of small, round blue cells with hyperchromatic nuclei and scant cytoplasm, features typical of Ewing sarcoma. Immunohistochemical staining was positive for CD99 (membranous) and FLI-1, with diff use nuclear positivity for NKX2.2 in a majority of tumor cells. Molecular testing (e.g., FISH or RT-PCR) confi rmed an EWSR1-FLI1 fusion, the canonical translocation seen in approximately 85- 90% of Ewing family tumors. The patient was referred to the Institute of Nuclear Medicine and Oncology, Lahore (INMOL) for further assessment.
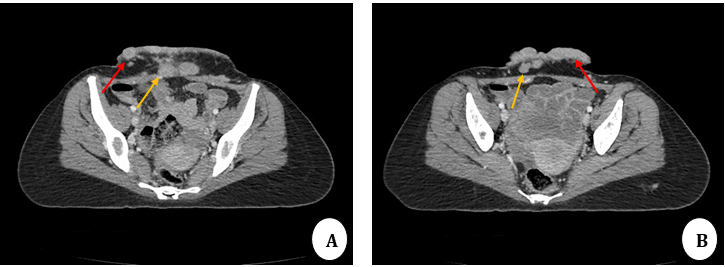
FIGURE 1 A & B: Contrast-enhanced CT scan axial images: Multiple enhancing cutaneous (red arrows) and subcutaneous nodules (yellow arrows) are noted in the lower anterior abdominal wall.

FIGURE 2: Contrast-enhanced CT scan axial images:
A: Multiple enhancing soft tissue lesions involving bilateral breasts (white arrows) – metastases
B: Lung window revealed subpleural soft tissue nodules on right side (red arrows) – metastasis
C: Hypodense lesion in the left hepatic lobe (yellow arrow) – metastasis
D: Bone window: Multiple lytic bony lesions ((green arrow) – metastases
Contrast-enhanced CT of the chest, abdomen, and pelvis revealed: 1. Multiple enhancing cutaneous and subcutaneous nodules in the lower anterior abdominal wall (Figure 1); 2. Bilateral multiple enhancing breast lesions with signifi cant internal vascularity on ultrasound (Figure 2A); 3. Bilateral pulmonary soft tissue nodules (Figure 2B); 4. A hypodense lesion in the left hepatic lobe (Figure 2C); and 5. Lytic lesions involving multiple bones (Figure 2D) findings consistent with metastatic spread.
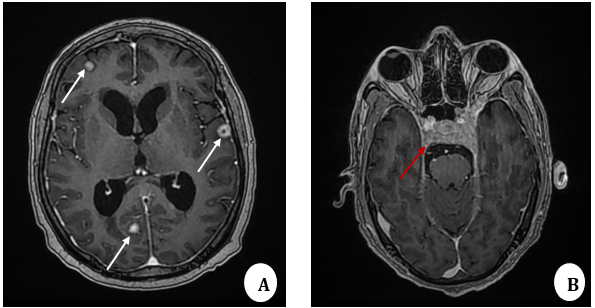
FIGURE 3: MRI brain T1W contrast-enhanced axial images:
A: Enhancing supratentorial soft tissue lesions (white arrows) – Brain metastatic
B: Bony metastatic lesion involving the clivus infi ltrating the left cavernous sinus (red arrow)
MRI brain was conducted due to neurological symptoms. Contrastenhanced MRI brain showed supratentorial brain parenchymal metastatic lesions (Figure 3A) and metastatic involvement of clivus extending into the left cavernous sinus (Figure 3B). Given the extensive systemic spread, surgical resection was not feasible. The patient was managed with systemic chemotherapy and palliative radiotherapy. The patient started systemic multiagent chemotherapy with the standard VAC/IE regimen, consisting of alternating cycles of Vincristine, Adriamycin, and Cyclophosphamide (VAC) with Ifosfamide and Etoposide (IE). Chemotherapy was delivered in an interval-compressed schedule every 2–3 weeks, as recommended in current Ewing sarcoma protocols (NCCN, COG, Euro-Ewing). In addition, palliative radiotherapy for osseous and brain lesions was initiated. Unfortunately, our patient could not bear chemotherapy and disease burden due to extensive disease and succumbed to her disease.
The Ewing sarcoma family comprises small round blue cell tumors characterized by specifi c chromosomal translocations. The most common translocation, t(11;22)(q24;q12), results in the EWSR1- FLI1 fusion gene, which promotes oncogenesis through aberrant transcriptional regulation.4
Although EES shares molecular features with osseous Ewing sarcoma, it diff ers in clinical presentation. Common anatomical sites for EES include soft tissues of the chest wall, paravertebral regions, and extremities such as the thighs and shoulders.5,6 Rare cases report involvement in the epidural space, subcutaneous tissues, and cervical foramina.7–9
Cutaneous manifestations, like in this case, are extremely rare and often misdiagnosed as benign dermatologic lesions, delaying diagnosis.10 The presence of symptoms during pregnancy in our case further complicate clinical recognition.
An intriguing aspect of this case is the timing of tumor progression during pregnancy and the postpartum period. Pregnancy-related hormones such as estrogen, progesterone, human chorionic gonadotropin, human placental lactogen, and growth hormone undergo dramatic fl uctuations, many of which are known to infl uence angiogenesis, cellular proliferation, and immune surveillance. Although the exact relationship between these hormonal changes and EES behavior remains uncertain, prior reports have noted rapid progression of Ewing sarcoma during pregnancy, raising the possibility of a hormonal contribution to tumor biology.14,15 In our patient, the unusually aggressive postpartum course could refl ect such hormonal infl uences, although coincidental progression consistent with the inherently aggressive nature of metastatic EES cannot be excluded. This case therefore underscores the importance of considering pregnancyrelated hormonal and immunological dynamics when interpreting tumor growth patterns in young women.
Metastasis from EES most frequently involves the lungs and bones, with respective rates of up to 80% and 40%.11 Brain metastasis is rare and typically portends poor prognosis. Similarly, breast involvement is exceedingly uncommon; only isolated case reports describe primary or metastatic EES to the breast tissue.12
Imaging is critical in evaluating disease burden. CT and MRI provide essential information for diagnosis, staging, and planning therapy.13 In this case, imaging was indispensable in identifying multiorgan involvement, including the central nervous system, thereby guiding palliative treatment.
Treatment of EES generally includes systemic chemotherapy, surgery, and radiotherapy. Prognosis is more favorable for localized disease. However, when metastasis is extensive, as in this patient, therapeutic goals shift toward symptom relief and quality of life improvement.
This case emphasizes the importance of considering Extraskeletal Ewing Sarcoma in the diff erential diagnosis of atypical or persistent skin nodules, particularly in young patients. Early biopsy and comprehensive imaging are crucial for timely diagnosis. The unique pattern of metastases in this case illustrates the aggressive nature of EES and highlights the essential role of radiology in patient management.
The authors declare no fi nancial support for the research, authorship, or publication of this article.
Conceptualization, Shahzad R; data acquisition, writing original draft, writing review and editing contributed by all authors. All authors have read and agreed to the published version of the manuscript.
The authors declare no conflict of interest.
Written informed consent has been obtained from the patient to publish this manuscript.