Journal of Case Reports and Reviews in Medicine (ISSN: 3069-0749)
Case Report Volume: 1 & Issue: 4
Case Report Volume: 1 & Issue: 4
Introduction: Aortic dissection is a rare but potentially catastrophic vascular emergency. It is characterized by an intimal tear of the aorta, leading to a false lumen that may cause complications. While the majority of ADs occur in the thoracic aorta, the ones confined to the abdominal aorta are extremely rare and present different diagnostic and management challenges due to atypical symptoms and delayed recognition. The risk factors for abdominal aortic dissections include hypertension, atherosclerosis, connective tissue disorders, trauma, and congenital anomalies. Using bedside POCUS in patients presenting with atypical pain may appropriately prompt additional imaging, including CTA, which is not typically pursued for shoulder pain. Timely diagnosis with modalities such as POCUS or CTA is crucial, as delayed recognition can lead to significantly higher morbidity and mortality.
This is a case of a 75-year-old female presenting with an extensive type B intramural hematoma extending to the para-visceral segment and a 5 cm infrarenal abdominal aortic aneurysm. It highlights the challenge in the management of this rare vascular pathology and underlines early recognition and multidisciplinary intervention as key to favorable outcomes.
Case Report: A 75-year-old female presented to the emergency department with sudden-onset back pain that began at 5:00 p.m. The pain was initially localized between her shoulder blades but progressively involved her entire spine. She also reported associated shortness of breath. Initial vital signs were significant for hypertension, with other parameters within normal limits. Physical examination revealed a patient in acute distress due to severe pain, but was otherwise unremarkable. This prompted bedside POCUS as part of the initial evaluation, which demonstrated findings concerning for an aortic aneurysm. A subsequent CTA obtained in the emergency department revealed an acute-on-chronic process with mural ulceration and likely penetrating atherosclerotic ulcers, with blood dissecting into the aortic wall.
Conclusion: The diagnosis of an aortic aneurysm is particularly concerning as it can lead to an aortic dissection which requires swift surgical intervention. Presentations can range from severe pain in the chest, upper back, or abdomen. The pain can radiate to the neck and shoulders. The two primary avenues for treatment include either surgical intervention, endovascular aortic repair, or medical management.
Keywords: Point-of-care Ultrasound, Infrarenal abdominal aortic aneurysm, back pain
An aortic dissection (AD) is a rare but life-threatening vascular emergency characterized by a tear in the intimal layer of the aorta, causing separation of the layers of the aortic wall which leads to creation of a false lumen. While aortic dissections are more commonly associated with the thoracic region, those confined to the abdominal aorta are rare events presented with unique diagnostic and therapeutic challenges due to atypical symptoms and often delayed clinical recognition.1 Primary abdominal aortic dissections account for less than 2% of cases, significantly lower compared to ascending aortic dissections (70%), descending aortic dissections (20%), and aortic arch dissections (7%).2
Abdominal aortic dissection symptoms include sudden onset abdominal or lower back pain, hypotension, or signs of ischemia in the lower limbs or visceral organs. The condition is often associated with underlying risk factors include hypertension, atherosclerosis, connective tissue disorders like Marfan syndrome and Ehlers-Danlos syndrome, and congenital anomalies such as bicuspid aortic valve, but it can also occur spontaneously or secondary to trauma or iatrogenic injury.3 Prompt diagnosis of abdominal aortic dissection is critical, as delayed intervention significantly increases morbidity and mortality. Computed tomography angiography (CTA) with IV contrast is the most common imaging modality used to diagnose and classify AD, and MRI can be used in case the use of CT or IV contrast is not desirable.4 Point-of-care ultrasound (POCUS) plays a critical role in the prompt bedside identification of aortic dissection, particularly prior to CT imaging or in settings where CT is not readily available. POCUS has demonstrated excellent diagnostic performance for abdominal aortic aneurysm (AAA) in the emergency department, with a reported sensitivity of 98% and specificity of 99%.7The initial approach to managing aortic dissection involves pain control, heart rate and blood pressure management, followed by surgical consultation.4
This case report details the presentation, diagnostic workup, and successful management of a 75 year-old female with an extensive type B intramural hematoma extending from the left subclavian artery to the para visceral segment, along with a 5 cm infrarenal abdominal aortic aneurysm (AAA). This case is significant as it demonstrates the complexity of managing a rare vascular pathology, highlighting the interplay between an extensive type B intramural hematoma and an infrarenal AAA. Early identification of the aneurysm using point-of-care ultrasound (POCUS) was essential, as it accelerated diagnostic clarity and facilitated timely escalation to definitive imaging and intervention.7 Given that the incidence of infrarenal AAAs in women over 65 is 1.7%6, this report underscores the importance of early recognition and multidisciplinary management in achieving a favorable outcome.
A 75-year-old female with a significant past medical history of hypothyroidism, and allergies to levothyroxine, presented to the emergency department with pain around her shoulder blades and shortness of breath. The patient described the pain as sudden in onset and denied any trauma to the back, heavy lifting, or physical activity. She denied any recent sickness, fevers, chills, chest pain, nausea, or diarrhea. On physical exam the patient appeared in acute distress and uncomfortable due to severe pain but otherwise her physical exam was unremarkable. Patients' vitals demonstrated hypertension, with initial blood pressure of 194/109. POCUS showed large aortic aneurysm (Figure 1). Computed tomographic angiography (CTA) of the chest demonstrated diffuse aortic wall abnormalities with extensive mural thrombus and irregular wall appearance (Figure 2). Areas of high attenuation within the aortic wall suggested the presence of blood products, indicating an acute on chronic process with mural ulceration and likely penetrating atherosclerotic aortic ulcers with blood dissecting into the aortic wall. Additionally, imaging revealed a large infrarenal abdominal aortic aneurysm measuring 5 cm, without evidence of rupture or extravasation. Patient was started on an esmolol drip, admitted to the ICU with consultation by Cardiothoracic surgery and Vascular surgery.
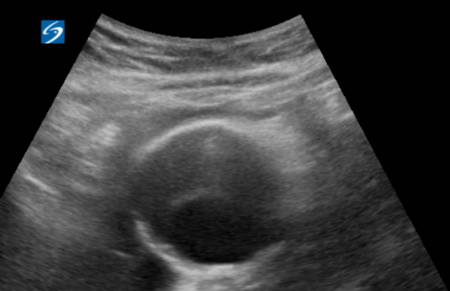
Figure 1. Point-of-care ultrasound demonstrating an infrarenal abdominal aortic aneurysm.

Figure 2. CTA image demonstrating extensive mural thrombus and a 5 cm infrarenal abdominal aortic aneurysm.
This case highlights several important aspects in the diagnosis and management of isolated abdominal aortic dissection (AAD), a rare variant of aortic dissection that presents unique clinical challenges.
From an emergency medicine standpoint, this case underscores the critical importance of maintaining a high index of suspicion for aortic dissection, even when patients present with nonspecific or atypical symptoms. Incorporating bedside POCUS as part of the initial evaluation particularly when the physical examination is non-specific can be invaluable. Early ultrasound assessment not only expedites recognition of life-threatening aortic pathology but also helps guide initial management decisions while definitive imaging, such as CT angiography, is being obtained. This approach enables earlier risk stratification, more timely consultation, and ultimately more rapid initiation of appropriate treatment. The patient's presentation with migratory back pain and shortness of breath represents a diagnostic challenge commonly faced in the emergency department, where the differential diagnosis is broad and time-critical decisions must be made quickly. Early recognition and rapid initiation of appropriate medical therapy in the emergency department are crucial steps that significantly impact patient outcomes.
The emergency physician’s role in this case exemplifies the importance of prompt recognition, immediate stabilization, and the judicious utilization of diagnostic imaging. Incorporating bedside POCUS as an early diagnostic adjunct played a significant role in accelerating clinical decision-making by identifying concerning aortic pathology prior to definitive imaging. This expedited pathway supported timely acquisition of CTA, which ultimately established the definitive diagnosis and enabled rapid initiation of medical management as well as appropriate specialist consultation. Early blood pressure control with esmolol and immediate critical care consultation demonstrate the essential components of initial emergency department management.
Medical management represents the cornerstone of treatment in uncomplicated type B dissections, with beta blockade being the primary intervention. The use of esmolol in this case exemplifies the importance of rapid blood pressure and heart rate control to reduce aortic wall stress and prevent progression. The goals of medical therapy include reducing heart rate below 60 beats per minute and maintaining systolic blood pressure between 100-120 mmHg. While beta blockers form the foundation of therapy, additional agents such as vasodilators may be necessary in some cases, though they should never be used without prior beta blockade.
The involvement of a multidisciplinary team, including emergency medicine physicians, radiologists, and cardiothoracic surgeons, underscores the importance of collaborative care in managing complex vascular pathologies. The successful outcome through medical management alone supports the growing evidence that not all type B dissections require immediate surgical intervention. However, this approach requires careful patient selection, close monitoring, and the availability of urgent surgical intervention if clinical deterioration occurs.
Long-term management typically involves transition to oral antihypertensive medications, regular imaging surveillance, and ongoing risk factor modification. This case adds to the limited literature on isolated abdominal aortic dissections and provides insights into the successful conservative management of complex aortic pathologies in elderly patients. Further research is needed to establish more definitive guidelines for managing patients with concurrent aortic dissection and aneurysmal disease, particularly in determining optimal timing and necessity of surgical intervention.
This case illustrates the successful management of a type B aortic dissection with concurrent infrarenal abdominal aortic aneurysm in an elderly patient. The favorable outcome in this case was achieved through prompt recognition in the emergency department, rapid initiation of medical therapy, and coordinated multidisciplinary care. The early use of bedside POCUS was a key factor in expediting diagnosis, allowing clinicians to identify the underlying aortic pathology far earlier than would have been possible with physical examination alone. This accelerated the diagnostic pathway, facilitated faster initiation of targeted treatment, and ultimately contributed to the successful clinical outcome.
The case emphasizes several key learning points: the importance of maintaining a high clinical suspicion for aortic dissection despite nonspecific presenting symptoms, the critical role of early bed side POCUS, CTA imaging in diagnosis, and the effectiveness of medical management in carefully selected patients with uncomplicated type B dissections.
The successful conservative management with beta blockade demonstrates that not all patients with type B dissections require immediate surgical intervention, particularly when there are no complications and the patient shows clinical stability. However, this approach necessitates close monitoring and readiness for surgical intervention if needed. The case also highlights the value of a coordinated approach between emergency medicine, critical care, and cardiothoracic surgery in managing complex vascular pathologies.
Moving forward, this case contributes to our understanding of managing concurrent aortic pathologies and supports the role of medical management in selected cases of type B aortic dissection. Further research and experience in this area will continue to refine our approach to these challenging vascular emergencies.
Disclosure: Authors have no current of past relationship with commercial entities.